A big drop in the number of patients turning up at accident and emergency (A&E) departments has prompted an unusual message from hospital bosses.
It’s ok to come to A&E if you need to, they said, and you won’t be waiting with patients suspected of having the covid-19 coronavirus.
The change of emphasis comes after years spent urging people to use alternatives to A&E unless they were genuinely suffering an emergency or had had a serious accident.
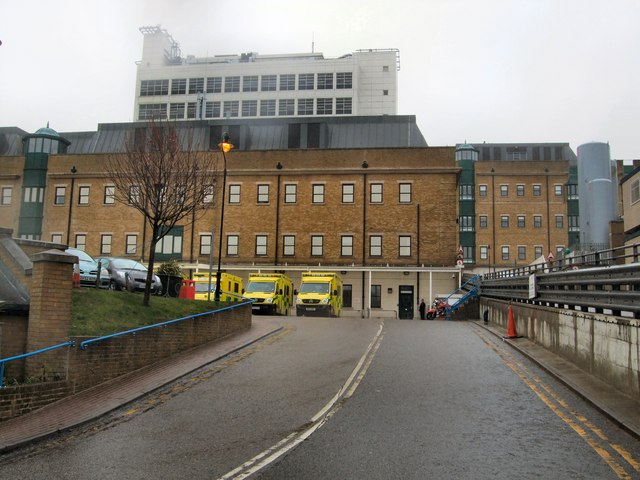
One of Britain’s leading emergency consultants, Rob Galloway, is currently the medical workforce lead for covid-19 at Brighton and Sussex University Hospitals (BSUH).
Dr Galloway said: “It’s still safe to attend A&E. If you need to come to A&E, you should.
“We’re concerned that the public are coming to harm because patients who are unwell aren’t coming to A&E.”
And when they did come, he said, they were often in a much more serious condition, with a poorer chance of survival or of making a good recovery.
A&E attendances and admissions at the Royal Sussex County Hospital, in Brighton, were almost 30 per cent down last month on March last year. The picture is similar across the country.
And nationally, the government reported a spike in the number of people dying – 6,000 more in one week than the five-year average.
Dr Galloway said that only about half of those were likely to be directly attributable to covid-19.
He said that there were some understandable reasons for the fall in A&E attendances – fewer people were going out drinking, fewer were driving and fewer were working.
And some of those who would be better off seeing their family doctor or a pharmacist were worried that they risked catching the coronavirus at A&E so were staying away.
But a third group of patients had also fuelled the drop in numbers at the emergency department.

Dr Galloway said that their reasons for not coming in included stoicism and selflessness, their fear of contracting the coronavirus and a worry that they might not receive the treatment they need as medics focus on patients with covid-19.
He said: “They may think that they’re helping the NHS but sadly they aren’t.”
When he and his colleagues finally got to see those patients, he said, they were sicker than they needed to be and required more care and treatment. This could mean a longer stay in hospital.
Their selflessness was admirable but misplaced and could partly explain the sudden spike in the number of people dying.
Dr Galloway said that A&E was safe, with red and green areas to separate patients suspected of having covid-19 from those with other conditions.
They would also be seen by entirely separate doctors and nurses. They were organised into teams of clinicians treating only coronavirus patients and teams treating all other patients.
It followed a huge reorganisation at BSUH, which runs the Royal Sussex and the Royal Alexandra Children’s Hospital, in Brighton, as well as the Princess Royal Hospital, in Haywards Heath, he said.
Dr Galloway said: “The public can be reassured we’re there for them whether they’ve got covid or something else.”
Staffing levels were good, he said, despite a number of colleagues who were off – some of them in self-isolation.
He said: “We’ve got resilience in A&E, the ward system and intensive care. We’ve got the capacity to cope.”
There were more than enough beds, he said. Occupancy rates were lower than they had been for years, partly thanks to a big drop in bed blocking, also known as “delayed transfers of care”.
He praised those working in social care, nursing homes and commissioning organisations for enabling more patients to be discharged more efficiently when they were ready to leave hospital, adding: “It’s remarkable.”
There were fewer “elective” patients too as many routine operations had been cancelled, along with outpatient appointments.
It worried him, though, that six months down the line there could be a rise in the number of, say, breast cancer cases coming to light.
There were fears that people were putting off seeing their doctor too when they had concerns about, say, a lump or other persistent or significant symptoms.
Dr Galloway also thanked everyone who had donated money, food or their time to help the NHS since the start of the pandemic.
And he thanked all those who had applauded NHS staff and carers, adding: “Those 8pm claps make you feel proud of working for the NHS.
“In films, heroes wear capes. In real life, heroes are people like nurses, radiographers, pharamacists and porters.
“It’s great that they feel appreciated. It’s a very hard job. It’s been the hardest couple of months of my working life and it’s wonderful that it’s appreciated.
“And it’s wonderful that the public are following the government’s advice about staying home and social distancing.
“Social isolation gave us an extra three weeks to prepare. We’re ready for you in A&E if you genuinely need us.
“If you can go to your GP or pharmacist, please do. But if it’s an emergency, come to A&E.
“If you’ve got abdominal or chest pain, loss of consciousness, fitting, heavy bleeding, if you’re having a stroke or breathing difficulties, don’t suffer at home and worry that you’ll be burdening us.
“If people are selfless, it may cause more problems for them and the NHS.
“The public can be reassured that we can cope.”